Breast cancer risk assessment is the new standard of care in women’s health — and effective breast cancer risk assessment tools play a critical role in ensuring women receive the individualized education and care they deserve. After all, breast cancer screening is no longer a one-size-fits-all approach. Instead, it should be personalized based on a woman’s unique breast cancer risk.
Recognizing the importance of early detection and personalized care
Risk Assessment ToolsHow Breast Cancer Risk Models Are Changing the Landscape for Young Women
According to a recently released report from the American Cancer Society (ACS), the rate of breast cancer among young women is rising. In Cancer Facts & Figures 2025, ACS says there is a concerning trend of increased breast cancer incidence — especially among women under 50. This increase is especially notable among women of color and those with a family history of breast cancer
“Invasive female breast cancer incidence has been increasing since the mid-2000s; from 2012 to 2021, the rate increased by 1% per year overall; 1.4% per year in women younger than 50 years; and by 0.7% in those 50 and older,” the organization says.
ACS notes that this trend is partly attributed to “changing risk factors, such as increased excess body weight, later age at first birth, and decreased number of childbirths.”
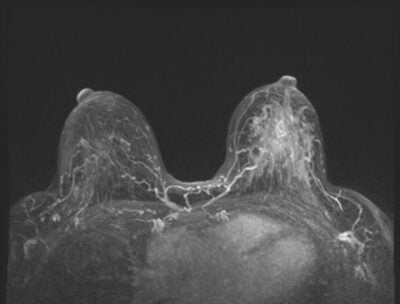
Breast cancer risk models use some of these factors to assess a patient’s risk. For instance, the popular Tyrer-Cuzick model analyzes data about a woman’s health and family background to produce a percentage-based score reflecting her breast cancer risk. The model uses a mathematical algorithm to combine multiple inputs, including genetic mutations, breast density, and extended family history.
New screening guidelines call for earlier risk assessment
With breast cancer rates rising among young women, it’s good news that updated breast cancer screening guidelines from the American College of Radiology® (ACR®) recommend that all women have a risk assessment by age 25 to determine whether they should start screening earlier than age 40. The ACR emphasizes that earlier screening is especially important for Black women and women of Ashkenazi Jewish heritage.
“The latest scientific evidence continues to point to earlier assessment as well as augmented and earlier-than-age-40 screening of many women — particularly Black women and other minority women,” says Debra Monticciolo, MD, FACR, primary author of the new guidelines and division chief, Breast Imaging, Massachusetts General Hospital, Boston. “These evidence-based updates should spur more-informed doctor-patient conversations and help providers save more lives.”
Why Luminary Risk is Crucial for Personalized Patient Education
Individualized patient education is a key part of these conversations, and MagView’s Luminary Risk is one of the most effective breast cancer risk tools to help you provide it. With Luminary Risk, you can seamlessly integrate the Tyrer-Cuzick, NCI, and BRCAPro risk models into your practice, ensuring your patients receive the most accurate and comprehensive risk score.
Plus, unlike free online tools, Luminary Risk provides a comprehensive breast screening care plan for your patients. This care plan includes a visual of the patient’s individualized risk — which educates and empowers patients as they work with you to create a personalized plan for breast cancer screening. As discussed in Why OBGYNs Need Breast Cancer Risk Tools to Identify High-Risk Patients, breast cancer risk assessment tools are increasingly vital for Obstetrics and Gynecology (OB-GYN) settings.




















![monitoring breast density shutterstock_1299510538-[Converted]](https://magview.com/wp-content/uploads/2023/05/shutterstock_1299510538-Converted.jpg)