In the U.S., approximately 1 in 8 women can expect to get breast cancer sometime during their lives. Since early detection is such a critical weapon in the fight against breast cancer, risk assessment is essential to help identify women who can benefit from more intensive breast cancer surveillance. Using breast cancer risk assessment models such as Tyrer-Cuzick in combination with a cutting-edge mammography reporting system is an effective way to do so. Within this process, radiologists are uniquely positioned to make a tremendous difference.
The unique role of radiologists in risk assessment
In a recent AuntMinnie article, Dr. Stacy Smith-Foley, the medical director of The Breast Center at CARTI, captured the important role of radiologists in breast cancer risk assessment.
“As a tenured radiologist, I feel that we, as radiologists, are uniquely positioned to assess and address hereditary cancer risk in women referred for breast imaging,” she wrote. “We can perform risk assessment for individuals sent for breast imaging using the information that has already been collected. Overall risk can also be addressed using models, such as Tyrer-Cuzick, and we have the tools to address hereditary cancer risk using national guideline criteria.”
As Dr. Smith-Foley noted, in a typical breast imaging setting, much of the information that is already collected from patients can be used to inform risk assessment. This is especially true for the Tyrer-Cuzick, which is one of the most popular breast cancer risk assessment models in use.
Understanding the Tyrer-Cuzick score
The Tyrer-Cuzick v8.0 (IBIS) estimates the likelihood of a woman developing breast cancer in 10 years and in her lifetime. It is considered “the most comprehensive” and “the most consistently accurate” model for predicting breast cancer risk, according to the American College of Radiology (ACR).
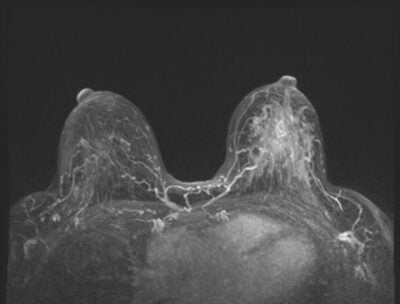
Tyrer-Cuzick uses various family factors, reproductive history, and overall medical history to estimate a patient’s breast cancer risk. Since breast density is a known factor that can increase the difficulty of detecting an abnormality and can also increase breast cancer risk, the Tyrer-Cuzick was updated in 2018 to include it in risk calculations.
According to Dense Breast-info, in the Tyrer-Cuzick model, “breast density is one of the top five factors determining breast cancer risk. This model is the most comprehensive and tends to be the most accurate at predicting risk at the population level.”
Integrating the Tyrer-Cuzick score into the radiologist’s workflow
One of the benefits of the Tyrer-Cuzick is that it is so comprehensive. However, if that much information is gathered and entered manually, the process can be very time-consuming.
The good news is that MagView offers an automated and time-saving approach to collecting the information, producing a risk score, and integrating it into the radiologist’s report.
There are three scenarios by which this happens:
- the structured reporting workflow
- the dictation only or hybrid workflow
- by using MagView’s new, stand-alone solution: Luminary Risk
Structured reporting workflow
In any of the following workflows, patients can fill out the required history information online from home, via a tablet in the waiting room, or through an interview with the technologist.
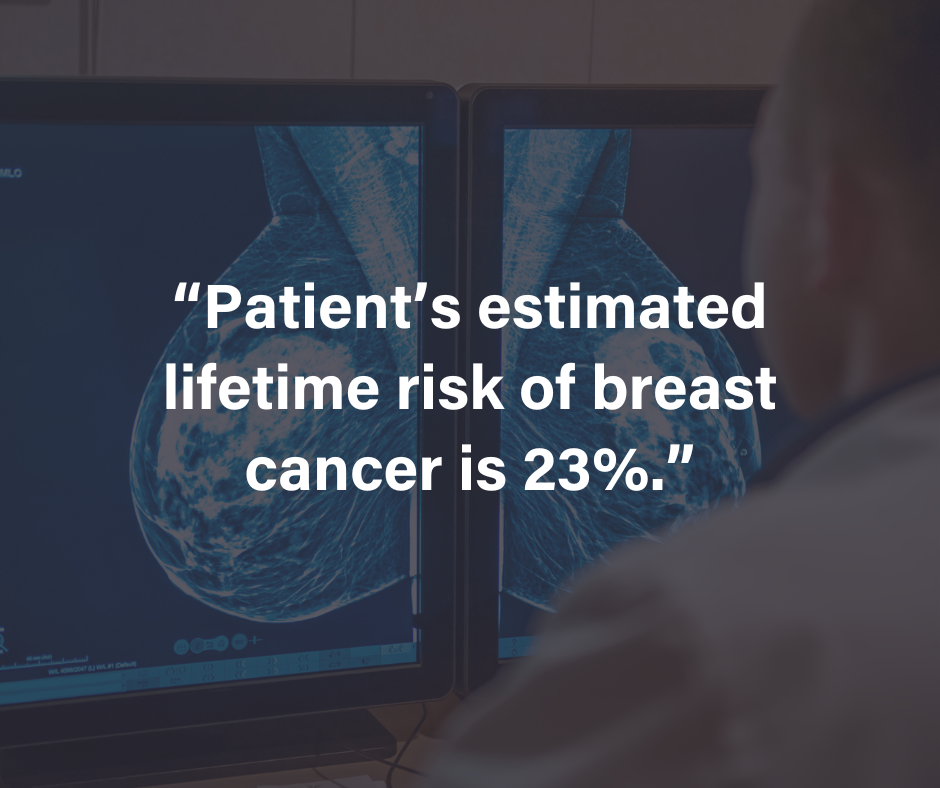
Once the information has been collected, MagView’s integrated Risk Assessment Module automatically calculates the risk for several risk assessment models—including Tyrer-Cuzick—based on electronic history and flags high-risk patients in a single system. The score is automatically inserted into the radiologist’s structured report without any additional button clicks.
MagView also provides real-time guidance and recommendations based on NCCN guidelines and/or a breast center’s custom protocol. Patients who are eligible for MRI, genetic testing, or genetic counseling are clearly identified. Plus—all recommendations are tracked to optimize follow-through.
In addition to the inclusion of the risk score in the radiologist’s final report, a custom risk letter can be automatically generated for the patient and/or referring provider.
Dictation only or Hybrid workflow
With a dictation only workflow in which sites are using dictation software, such as PowerScribe 360®, the process is the same. However, the history narrative, Tyrer-Cuzick score, and recommendations statement are automatically inserted into the dictation software’s report. A hybrid workflow is a combination of dictation and structured reporting. The risk score automatically populates in both types of reports in this workflow.
New: Luminary Risk
Luminary Risk is a new and stand-alone risk assessment solution that provides facilities without MagView’s tracking and reporting system a dedicated risk assessment tool — which includes the Tyrer-Cuzick model.
Developed in response to the limitations of EHR systems in assessing breast cancer risk, Luminary Risk provides breast imaging centers with an integrated and comprehensive solution for assessing patients’ risk for breast cancer.
Luminary Risk seamlessly integrates with existing EHR systems to optimize the delivery of personalized high-risk breast screening to patients. This integration enhances high-risk screening programs by eliminating cross-platform manual data entry and providing healthcare providers with readily available risk assessment results without disrupting established workflows.
In an “EHR driven” workflow, history can be collected one of two ways:
- Via Luminary Risk tools such as a tablet in the waiting room or via an interview with the technologist via TechPad.
- Via the established history collection within EMR.
Once the risk score is generated, it will be sent to the patient’s chart in EMR to be accessible by the radiologist. That score can be manually dictated into the radiologists report or automatically inserted via our dictation integration.
Breast imaging in the era of personalized care
In our recent webinar, “Breast Imaging in the Era of Personalized Care: Tools, Tactics, and Triumphs in Risk Assessment” Dr. Smith-Foley discussed an array of topics — including the importance of risk assessment and its value for your patients and your practice.
“The primary goal of risk assessment is to help health care professionals estimate a patient’s risk of developing breast cancer,” Dr. Smith-Foley said. “Performing risk assessment adds value to the yearly screening exam and allows the radiologist to provide recommendations specifically selected for an individual patient based on their family history.”
“Many of the patients seen in a breast center are smart, savvy healthcare consumers looking not only for the latest technology and a good experience, but also for the most up- to date recommendations,” she added. “There is no longer a one-size-fits-all solution.”
Using breast cancer risk assessment models such as Tyrer-Cuzick has become best practice in breast cancer screening. Doing so supports early detection efforts and can help identify patients who can benefit from a personalized screening approach. By using MagView’s structured reporting and risk assessment software together, you can boost your center’s efficiency and optimize radiologists’ workflow.
If you’d like to see MagView’s risk assessment platform in action, please request a demo today.












![monitoring breast density shutterstock_1299510538-[Converted]](https://magview.com/wp-content/uploads/2023/05/shutterstock_1299510538-Converted.jpg)