When it comes to risk assessment for breast cancer, many experts underscore the importance of screening early enough and often enough using the most appropriate screening modality. In a recent update to its breast cancer screening recommendations, the American College of Radiology® (ACR®) now recommends that women have their breast cancer risk assessed by age 25.
But the ACR isn’t the only organization putting forth new recommendations — the U.S. Preventive Services Task Force (USPSTF) recently posted a new draft recommendation about breast cancer screening, too.
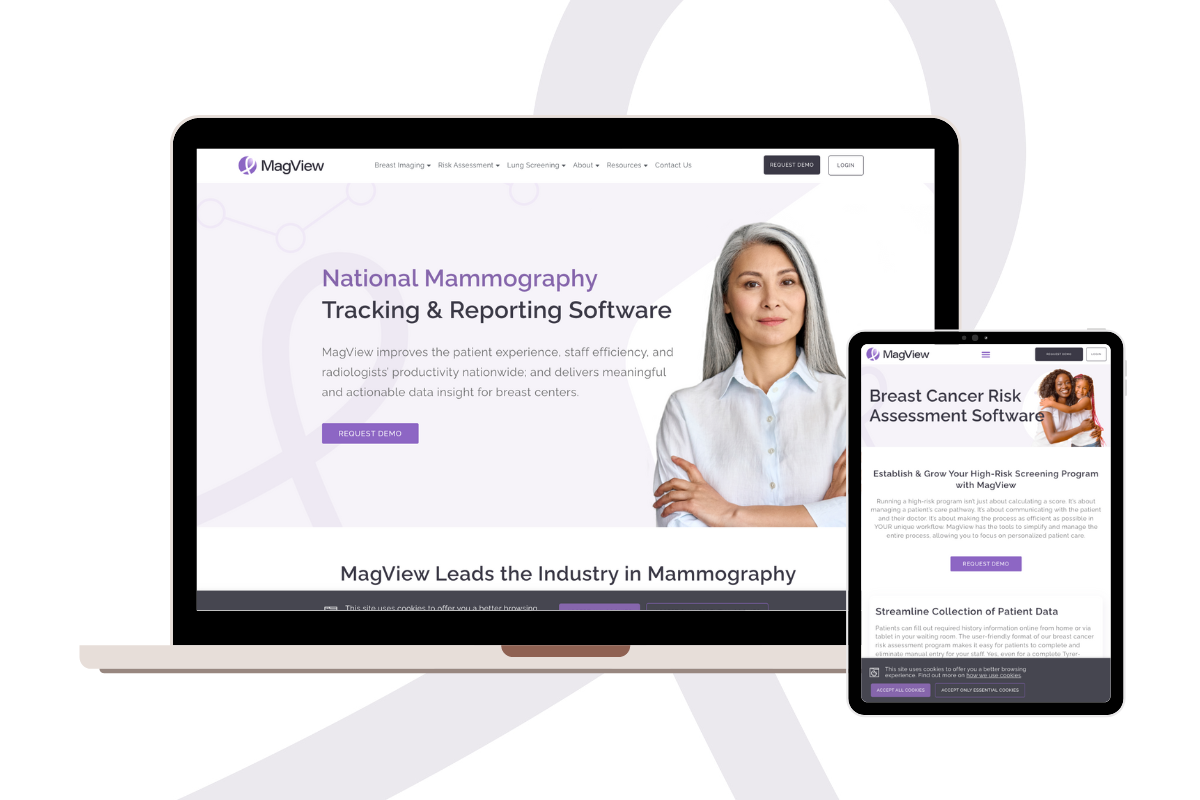
Here, we’ll take a look at both — as well as how MagView’s risk assessment tool for breast cancer can help your breast center ensure that patients are receiving the precise screening they need.
Get expert workflow tips and more delivered to your inbox monthly.
Risk Assessment for Breast Cancer: ACR Screening Guidelines Updated
On May 4, the ACR announced that it had issued new breast cancer screening guidelines which recommend that all women have a risk assessment by age 25 to determine whether they should start screening earlier than age 40. The ACR emphasized that earlier screening is especially important for Black women and women of Ashkenazi Jewish heritage.
“The ACR continues to recommend annual screening starting at age 40 for women of average risk, but earlier and more intensive screening for high-risk patients,” according to the announcement, which also noted that the new ACR guidelines for high-risk women were published online May 3 in the Journal of the American College of Radiology (JACR).
Additional updates to the new ACR breast cancer screening guidelines include:
- “Women with genetics-based increased risk (including BRCA1 carriers), those with a calculated lifetime risk of 20% or more and those exposed to chest radiation at a young age are recommended to have MRI surveillance starting at ages 25 to 30. These women should start annual mammography at ages 25 to 40, depending on type of risk.”
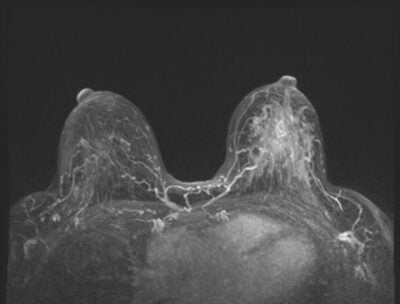
- “Women diagnosed with breast cancer prior to age 50 or with personal history of breast cancer and dense breasts should have annual supplemental breast MRI.”
- “High-risk women who desire supplemental screening — but cannot undergo MRI screening — should consider contrast-enhanced mammography (CEM).”
Advantages of Early Detection
“The latest scientific evidence continues to point to earlier assessment as well as augmented and earlier-than-age-40 screening of many women — particularly Black women and other minority women,” said Debra Monticciolo, MD, FACR, primary author of the new guidelines and division chief, Breast Imaging, Massachusetts General Hospital, Boston. “These evidence-based updates should spur more-informed doctor-patient conversations and help providers save more lives.”
Risk Factors: Race & Prevalence
The announcement said the ACR’s reclassification of Black women and other minorities to high-risk was based on a variety of factors, including the fact that, compared to non-Hispanic white women:
- Minority women under age 50 are: “127% more likely to die of breast cancer; 72% more likely to be diagnosed with breast cancer; and 58% more likely to be diagnosed with advanced-stage breast cancer.”
- Black women are “42% more likely to die from breast cancer despite roughly equal incidence rates.”
- Black women are “less likely to be diagnosed with stage I breast cancer but twice as likely to die of early breast cancers.”
- Black women have “a two-fold higher risk of aggressive — ‘triple-negative’ — breast tumors and a higher risk of BRCA1 and BRCA2 genetic mutations (placing them at higher risk).”
“Since 1990, breast cancer death rates in Black women, who develop and die from the disease earlier, have only dropped approximately half as fast as in white women,” said Stamatia Destounis, MD, FACR, co-author of the new guidelines, chair of the American College of Radiology Breast Imaging Commission and managing partner at Elizabeth Wende Breast Care in Rochester, NY. “We continue to regularly examine the latest evidence and update our recommendations to help save more Black women and others at high risk from this deadly disease.”
Take home points from the new ACR guidelines provide a bit more detail, as well as a summary of the changes:
- “All women should have risk assessment by age 25, especially black women and women of Ashkenazi Jewish heritage.”
- “For most women at higher-than-average risk, the supplemental screening method of choice is breast MRI. For those who qualify for but cannot undergo breast MRI, CEM or US could be considered.”
- “Women with genetic mutations (and their untested first-degree relatives) or those with a calculated life-time risk of 20% or more should have annual DM, with or without DBT, starting at age 30 and annual MRI starting age 25 to 30. Mutation carriers can delay mammographic screening until age 40 if annual breast MRI is performed as recommended. Women exposed to a cumulative chest RT dose of >/= 10Gy by age 30 should have annual mammography starting at age 25 or 8 years after RT, whichever is later, and annual breast MRI beginning at age 25-30.”
- “Women diagnosed with breast cancer prior to age 50 or with a personal history (PH) of breast cancer and dense breasts should have annual supplemental screening with breast MRI. Others with PH should strongly consider supplemental screening with MRI, especially if other risk factors are present.”
- “For women with dense breasts who desire supplemental screening, breast MRI is recommended. Women with atypia or LCIS, should consider supplemental surveillance with MRI, especially if other risk factors are present.”
USPSTF’s Proposed Changes Do Not Include Breast Cancer Risk Assessment
Several days after the ACR announcement, the U.S. Preventive Services Task Force (USPSTF) announced some proposed changes of its own.
On May 9, the USPSTF posted a draft recommendation statement on screening for breast cancer recommending that all women get screened for breast cancer every other year starting at age 40 — which is a decade earlier than the USPSTF previously recommended.
Unlike the detailed recommendations made by the ACR, the recommendations made by the Task Force:
- Are only geared toward average-risk women
- Do not include recommendations for breast cancer risk assessment
- Do not address the screening needs of patients with dense breasts
- Continue to recommend biannual, rather than annual screening
And while the USPSTF also addressed the greater impact of breast cancer on Black women, the draft recommendations call for more research in this area, rather than the specific recommendations made by the ACR — which considers Black women and other minorities to be at high risk.
The Task Force’s draft recommendation statement, draft evidence review, and draft modeling report were posted for public comments, which closed on June 5. Once comments have been reviewed and considered, the Task Force will issue its final recommendation.
Breast Cancer Risk Calculator
In its coverage of the USPSTF’s new breast cancer screening recommendations, the Breast Cancer Research Foundation (BCRF) addressed the lack of consensus on screening guidelines and the “critical need to move from an age-based approach to breast cancer screening to a personalized, risk-based approach.”
“Coupling a risk-based model with improved screening technologies…has the power to drastically improve early detection,” the BCRF said.
“I am so excited that we’re at a point in medical history where we have new tools to finally move from a very crude, imprecise, age-based screening for breast cancer to the precision of risk-based screening to detect breast cancer,” BCRF investigator Dr. Connie Lehman said. “It’s unbelievable that we have this opportunity now. But we have a lot of work to do to actually get women on a risk-based protocol.”
How to be Proactive
The good news is that MagView’s risk assessment solution can help your breast center ensure that each woman receives the precision screening she deserves. Breast cancer risk models within MagView help you categorize a woman’s risk of breast cancer using her personal and familial medical history.
In addition to our online Tyrer-Cuzick Risk Assessment Calculator geared for patient use, MagView’s breast cancer risk assessment software gives your breast center the ability to integrate automated risk assessment into your workflow.
With MagView’s breast cancer risk assessment software, you can:
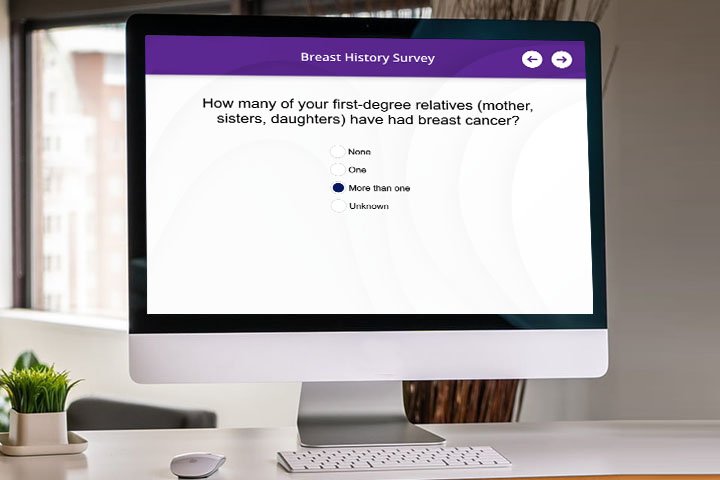
- Streamline collection of patient data: Patients can fill out required history information online from home or via tablet in your waiting room. The user-friendly format of our breast cancer risk assessment program makes it easy for patients to complete and eliminates manual entry for your staff. Yes, even for a complete Tyrer-Cuzick v8.0 (IBIS) assessment!
- Automatically identify “high-risk” patients: There is no need to log into another system or website. MagView automatically calculates the risk assessment score and flags high-risk patients in a single system. Integrate the score into your radiologist’s reporting platform with no interruption to their workflow.
- Incorporate genetic testing: MagView provides real-time guidance and recommendations based on NCCN guidelines and/or your organization’s custom protocol. Patients eligible for MRI, genetic testing or genetic counseling are clearly flagged. Each recommendation is tracked to ensure follow-through. Integrations with genetic testing labs, such as Myriad, allow you to deliver comprehensive risk assessment without burdening your staff with additional paperwork.
- Communicate risk information to patient and provider: Risk score and recommendation (such as breast MRI) can be included in the radiologist’s imaging report with no additional steps. Automatically communicate risk score and personalized recommendations to the patient and provider. MagView provides options to integrate with breast density measurement software for risk calculation and density notification to the patient and provider.
- Automate patient follow-up: MagView takes the burden off your staff by automatically generating reminder letters, text messages, and emails to patients. Our automated follow-up tools boost patient return rates.
To learn more about how MagView can help your breast center offer risk assessment for breast cancer, please contact us.












![monitoring breast density shutterstock_1299510538-[Converted]](https://magview.com/wp-content/uploads/2023/05/shutterstock_1299510538-Converted.jpg)