When it comes to breast cancer risk, breast density is a known factor that can increase the difficulty of detecting an abnormality. For this reason, 38 states and the District of Columbia currently require some type of breast density notification after a mammogram. There is also legislation in the works to enact similar dense breast notification (DBN) requirements at the federal level.
With that much discussion about the role of breast density, one may assume that those within the breast imaging industry are well-versed about best practices for conducting thorough evaluation and follow-up in this context. However, a recently-published study reveals this may not be the case. Here, we’ll examine study results and offer a few recommendations for addressing them.
What knowledge gaps were identified in the study?
The study, “Radiologic Technologist and Radiologist Knowledge Gaps about Breast Density Revealed by an Online Continuing Education Course,” was published in the July/August 2020 issue of the Journal of Breast Imaging. It made use of a breast density continuing education course marketed to the radiology community to assess “provider knowledge gaps and their predictors.”
Of the 1649 registrants whose responses could be analyzed:
- 82% were radiologic technologists.
- 7% were physicians.
- 6% were nonphysicians.
Of those who were physicians and radiologic technologists, over 90 percent in each category specialized in radiology.
What knowledge gaps were identified in the study? The authors describe them as those related to:
- Breast density
- Breast cancer risk assessment
- Breast cancer screening
Such findings underscore the need for a more focused approach to understanding the implications of breast density—as well as the appropriate application of risk models and risk-based screening.
Why is breast density important in breast cancer screening?
As cited in the study, breast density is important in breast cancer screening, since:
- Increasing breast density can make it more difficult to detect cancer.
- Mammographic sensitivity is reduced 50-60% in women who have extremely dense breasts.
- Women with extremely dense breasts vs those with fatty breasts face a much higher risk.
Despite these factors, the authors note that “40%–87% of patients are unaware of the associated increase in breast cancer risk with increasing breast density” and 49%–92% of physicians ordering mammograms are only “somewhat comfortable” talking about breast density with patients and its associated implications.
Which risk models most effectively integrate breast density factors?
Risk models are used to identify patients who fall into specific risk categories to better guide individualized screening and surveillance planning for clinical management. Some models are used to determine whether a woman is generally at high risk. Others have more specific applications, such as identifying women who may:
- Benefit from risk-reducing medications.
- Carry a pathogenic mutation in BRCA1 or BRCA2.
- Meet criteria for high-risk screening MRI.
Although risk models can be quite helpful, they’re not always accurately applied to a patient’s specific situation. For example, in the breast density study, results indicated that nearly 33% of physicians and 34% of technologists/nonphysicians incorrectly believed the Gail model should be used to identify high-risk patients to determine whether MRI or genetic testing should be recommended.
However, according to DenseBreast-info, Inc. (the source of course information for the study), neither the Gail model nor the Penn II or Clause models include breast density risk calculations.
Models which do include them are:
- Tyrer-Cuzick Model (IBIS) version 8: “In this model, breast density is one of the top five factors determining breast cancer risk. This model is the most comprehensive and tends to be the most accurate at predicting risk at the population level.”
- Breast Cancer Surveillance Consortium (BCSC) model: “A modification of the Gail model…includes the risk factors with the greatest population attributable risks for breast cancer, including age, breast density, family history, history of a breast biopsy, and a polygenic risk score (PRS) based on common genetic variations.”
Additionally, the organization notes that artificial intelligence (AI) is also starting to play a role, since it’s “being used to identify textural and other findings beyond breast density on mammograms that predict increased risk; such information is complementary to the Tyrer-Cuzick model (v.8).”
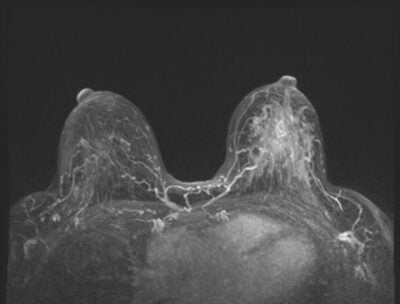
Which risk-based screening modalities are most appropriate?
The goal of risk-based screening is to “reduce the number of women who are screened or the frequency of screening or both.” Of course, it also helps to ensure the use of the most appropriate screening modalities for those with specific high-risk factors. Again, the study revealed this may not always occur.
Results demonstrated that 31% of physicians and nearly 48% of technologists/nonphysicians were “unaware that MRI should be recommended for women with a family history of BRCA1/BRCA2 mutations.” Additionally, participants overestimated the effectiveness of tomosynthesis, with 30% of physicians and nearly 35% of technologists/nonphysicians “believing sensitivity nearly equaled MRI.”
DenseBreast-info, Inc. provides a summary of screening modalities and how they should be applied, as well as a Screening Decision Support Tool. Together, they provide a comprehensive framework to help providers select the most appropriate diagnostic path for each patient’s unique needs.
How can breast centers work to improve these gaps?
By 2022, it’s anticipated that the U.S. Food and Drug Administration (FDA) will enact “landmark policy changes to modernize mammography services and improve their quality”—including a requirement for breast density reporting and an enhanced ability for the FDA “to enforce mammography facilities’ compliance with standards.”
To both optimize patient care and prepare for these changes, it is essential that the knowledge gaps about breast density be reduced—which can be accomplished through ongoing education. The importance of this dynamic is highlighted in one of the “key messages” provided as a takeaway from the study:
“These knowledge gaps, particularly among physicians, may lead to the underutilization of comprehensive risk assessment and the underuse of screening MRI in women at high risk. Continued development of targeted, medically-sourced educational resources to facilitate well-informed shared decision making between patients and providers is important to ensure patients are recommended for appropriate breast cancer screening.”
In this light, the nonprofit DenseBreast-info, Inc. is one resource that can help. Its website was launched in April 2015 to provide “comprehensive, peer-reviewed, medically-sourced information to patients and health care providers about breast density and the impact of dense breasts (heterogeneously dense or extremely dense) on breast cancer screening and risk, including considerations for supplemental screening based on breast density and/or other risk factors.”
There are additional breast density websites that offer information for both patients and referring providers, which can be found in a list provided by the Society of Breast Imaging and compiled by Jennifer Harvey, MD, FACR, FSBI, who is one of many scientific advisors for DenseBreast-info, Inc.
Another important way breast centers can improve these gaps is by partnering with a state-of-the art mammography reporting system that offers software solutions that align with the latest MQSA regulations and are delivered through a platform that offers a variety of cutting-edge tools. These tools should support optimal patient care while making life easier for patients, clinicians, and the breast centers who support them.
MagView is such a partner, and we can provide the support you need to ensure excellence in patient care and adherence to compliance within an evolving regulatory landscape.
For information on risk models and tips for implementing risk-based screening at your practice, click here.
For information on how to automatically incorporate automated breast density in your radiology report, click here.
Contact us today to learn more.



















![monitoring breast density shutterstock_1299510538-[Converted]](https://magview.com/wp-content/uploads/2023/05/shutterstock_1299510538-Converted.jpg)