Many breast imaging centers have opened high-risk screening clinics to augment their existing services. This has already become the new standard, as organizations look for justification to expand patient services, recommend breast MRI screening exams, and providing referrals for genetic counseling.
Preventative care and increasing downstream revenue are the major factors in the decision for many sites to implement or enhance their existing high-risk programs. Another factor to consider, however, is that offering a service dedicated to screening patients for high risk, without the proper tools, can put more stress on the breast imaging workflow.
The problem is that many systems are not set up to function on this plane. Subsequently, some sites resort to manual data entry on risk model websites to calculate each score individually. Calculated risk models, such as Tyrer-Cuzick and the Gail Model, are simply not built into the RIS mammography tracking module, mammography information system, or EMR module.
Some programs offer standalone, web-based risk platforms only, although this method adds to system fragmentation, redundancy, and increased room for error. This is especially true when the reader wants to add the risk score to their finding report, or if the site wants to include risk-related information in the patient notification letter.

The Tyrer Cuzick App
Tyrer-Cuzick version 8 has 25 elements and family history factors alone, so the time required to enter this for every patient, every study, and every day adds up fast. In most cases, the facility is already required to enter this information into their existing mammography tracking solution and, in order to generate the risk score, that same information has to be re-entered into an online calculator.
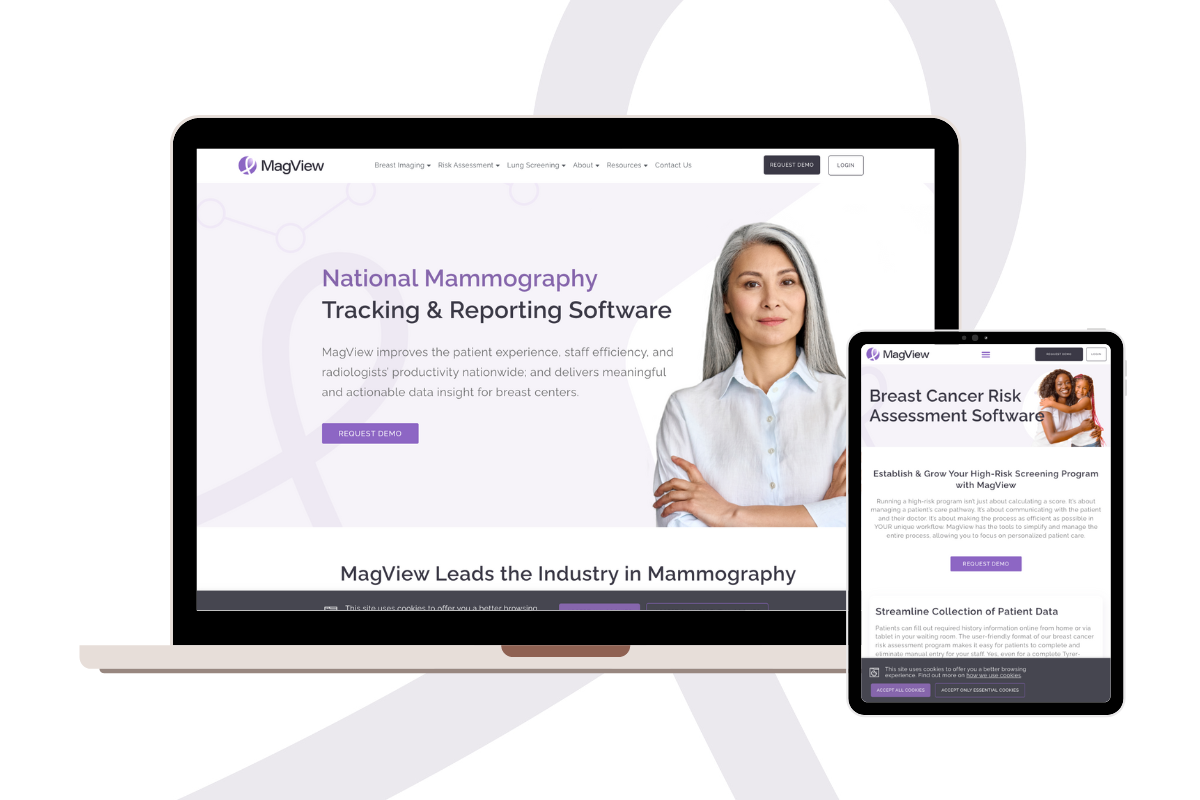
One provider, however, has considered this workflow and incorporated several breast cancer risk models into their base program. MagView offers automated calculations for all available risk models, such as Tyrer-Cuzick, Gail, BRCAPro, and Claus. In their program, patients can enter breast cancer risk factors in advance of the appointment using a patient history portal, saving the facility staff countless hours a day. The patients can also use the patient history tablet module for electronic submission to the breast center and MagView system.
These factors are saved from year to year, so the patient only needs to modify any changes in the previous history on subsequent visits. The calculators are built into the program, so no external websites or third-party programs are needed. The data is then used in the automatic risk calculation, and the radiologists can see the score in real-time, affecting their decision on follow-up recommendation. Scores can automatically be included in the finding reports, saving the readers additional time, and patients can be notified with automated text inserted into the letter based on their score.

Evidence has shown that including risk information in both the finding reports and patient letters has increased awareness along all fronts, especially when qualifying patients for additional imaging, like breast MRIs. One site reported a 100% increase in breast MRI referrals from their previous workflow using their RIS mammography tracking module as a reporting tool. Another site in Georgia reported a 106% increase in MR referrals, resulting in $80,000 in additional annual revenue.
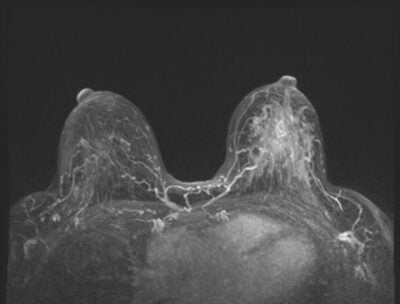
Beyond the financial benefits, the bottom line is, increased high risk screening has improved the detection of cancers by ensuring patients who are at a high risk receive the care and additional imaging they need. In a recent study of BRCA mutation carriers and women of 20% or higher lifetime risk for breast cancer, sensitivity for breast cancer detection was 90.0% using MRI versus 37.5% for mammography and 37.5% for ultrasound (Source: Journal of Clinical Oncology. 2015;33(10):1128-35).
For more information about MagView and their high-risk program solutions, visit: https://magview.com/breast-cancer-risk-assessment
















![monitoring breast density shutterstock_1299510538-[Converted]](https://magview.com/wp-content/uploads/2023/05/shutterstock_1299510538-Converted.jpg)